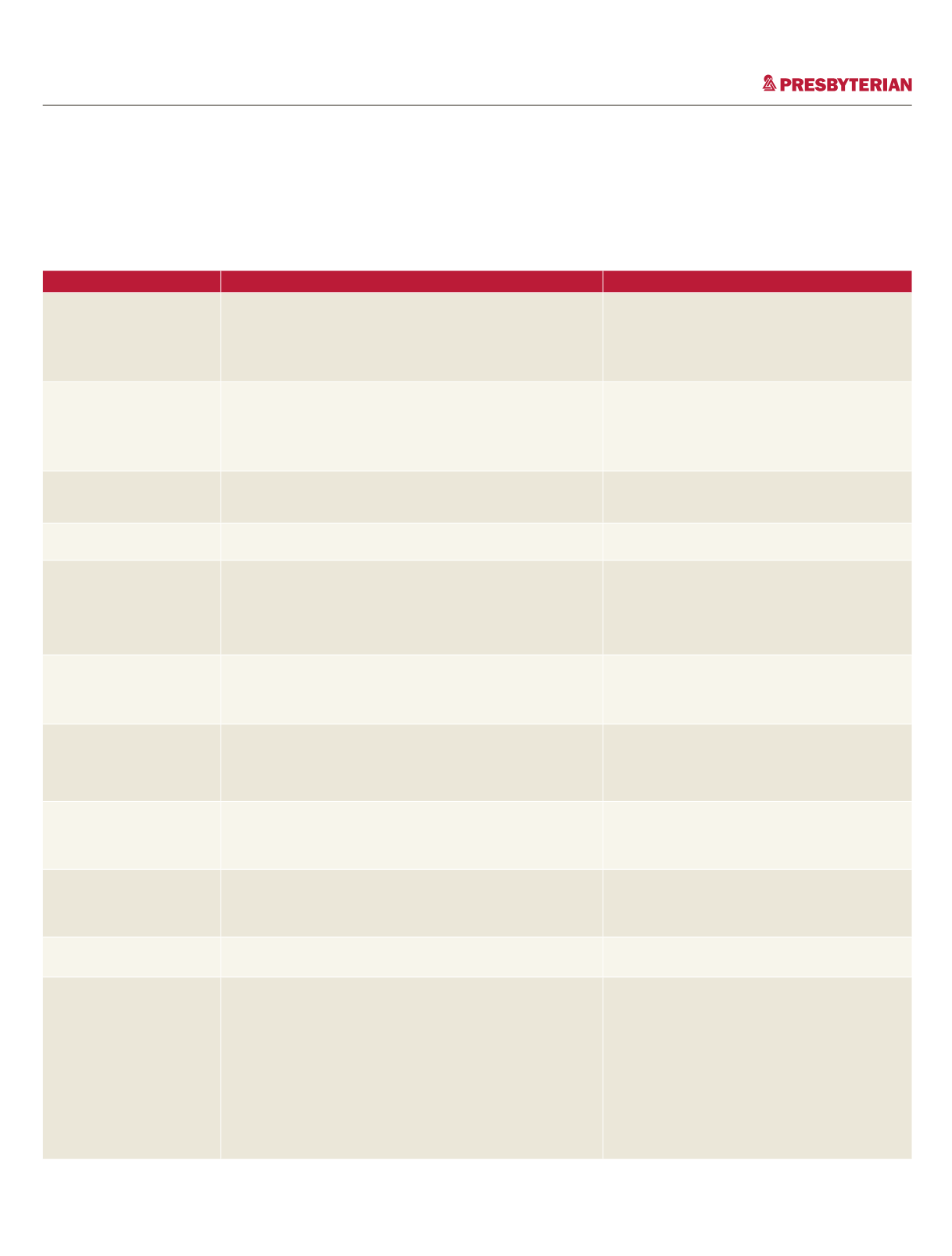
2016 Medicare preventive services
A guide for members
This educational tool provides information on Medicare preventive services.
6
Service
Who is covered
Frequency
Initial Preventive Physical
Examination (IPPE). Also
known as the “Welcome
to Medicare Preventive
Visit”
All new Medicare beneficiaries who are within the first
12 months of their Medicare Part B coverage period.
Important—The screening EKG is an optional service that may
be performed as a result of a referral from an IPPE.
■
Once in a lifetime
■
Must furnish no later than 12 months after the
effective date of the first Medicare Part B
coverage
Annual Wellness Visit
(AWV)
All Medicare beneficiaries who are no longer within 12 months
after the effective date of their first Medicare Part B coverage
period and who have not received an IPPE or AWV within the
past 12 months.
■
An initial visit, once in a lifetime
■
Subsequent visits, annually
Ultrasound Screening for
Abdominal Aortic
Aneurysm (AAA)
Medicare beneficiaries with certain risk factors for AAA and
who receive a referral from their physician, physician assistant,
nurse practitioner, or clinical nurse specialist.
Once in a lifetime.
Cardiovascular Screening
Blood Tests
All Medicare beneficiaries without apparent signs or
symptoms of cardiovascular disease.
Every 5 years.
Diabetes Screening Tests
Medicare beneficiaries with certain risk factors for diabetes or
diagnosed with pre-diabetes.
Beneficiaries previously diagnosed with diabetes are not
eligible for this benefit.
■
Two screening tests per year for beneficiaries
diagnosed with pre-diabetes
■
One screening per year if previously tested, but
not diagnosed with pre-diabetes, or if never
tested
Diabetes Self-
Management Training
(DSMT)
Medicare beneficiaries diagnosed with diabetes.
Physician or qualified non-physician practitioner treating the
beneficiary’s diabetes must order DSMT.
■
Up to 10 hours of initial training within a
continuous 12-month period.
■
Subsequent years: Up to 2 hours of follow-up
training each year after the initial year
Medical Nutrition Therapy
(MNT)
Certain Medicare beneficiaries diagnosed with diabetes or
renal disease, or who have received a kidney transplant within
the last 3 years.
A registered dietitian or nutrition professional must provide
the services.
■
First year: 3 hours of one-on-one counseling
■
Subsequent years: 2 hours
Screening Pap Tests
All female Medicare beneficiaries.
■
Annually if at high risk for developing cervical or
vaginal cancer, or childbearing age with
abnormal Pap test within past 3 years
■
Every 24 months for all other women
Screening Pelvic
Examinations
All female Medicare beneficiaries.
■
Annually if at high risk for developing cervical or
vaginal cancer, or childbearing age with
abnormal Pap test within past 3 years
■
Every 24 months for all other women
Screening Mammography
All female Medicare beneficiaries aged 35 and older.
■
Aged 35 through 39: One baseline
■
Aged 40 and older: Annually
Bone Mass Measurements
Certain Medicare beneficiaries that fall into at least one of the
following categories:
■
Women determined by their physician or qualified non-
physician practitioner to be estrogen deficient and at clinical
risk for osteoporosis;
■
Individuals with vertebral abnormalities;
■
Individuals receiving (or expecting to receive) glucocorticoid
therapy for more than 3 months;
■
Individuals with primary hyperparathyroidism; or
■
Individuals being monitored to assess response to FDA-
approved osteoporosis drug therapy
■
Every 24 months
■
More frequently if medically necessary
















